Mammography
Mammography is the primary imaging modality for early detection of breast cancer. Mammography may detect cancer 2-4 years earlier before a cancer becomes clinically evident. There are many new advancement in mammography made over years to improve the image quality as well as reduce radiation dose in order to provide earlier diagnosis of breast disease, more accurate assessment of disease extent and improve detection of recurrence.

Screening mammography is used to detect breast cancer in women who have no signs or symptoms of the disease.
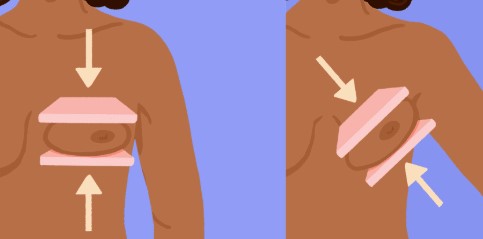
Mammography Views
It involves taking x-ray of the breasts in 2 views annually or biennially following recommended guidelines.
- MLO view (medial lateral oblique view)
- CC view (cranial-caudal view)
A very small doses of radiation are used and risk of harm from this radiation exposure is low.
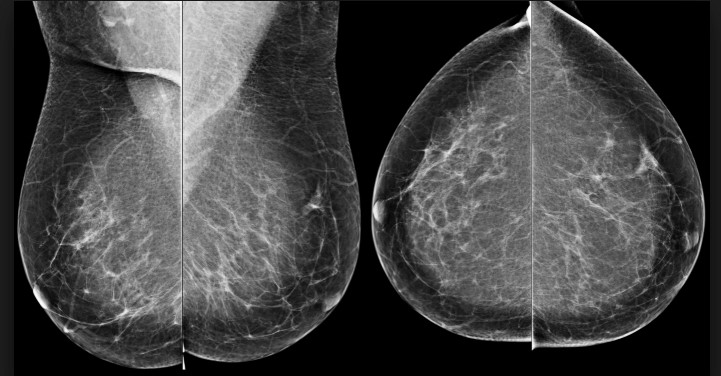
MMG – MLO view MMG – CC view
MMG – CC view MMG – MLO view
Breast Density and Mammographic Report
Younger women and women of Asian ethnicity are know to have dense breast.
Breast density is due to the breast having more fibrous and glandular tissue and less fatty tissue in the breasts.
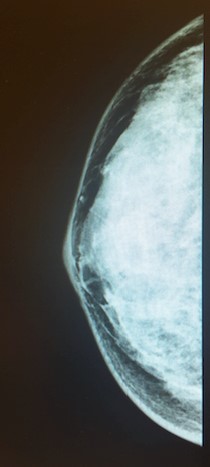
Dense breast – more “white”
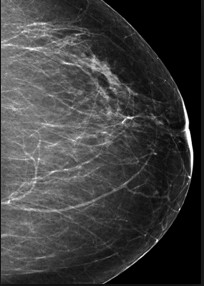
Fatty breast – more “black” on MMG
Abnormality on Mammography
Any area that are suspicious and does not look like normal breast tissue eg.
- Areas of significant opacity, increased density
- Small white dots / spots in clusters known as microcalcifications
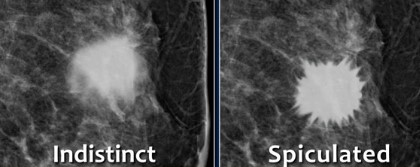
- Irregular, indistinct and spiculated margins of the mass
- Loss of normal breast architecture.
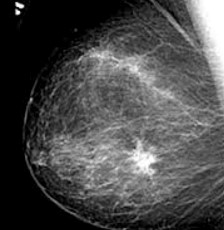
Suspicious mass are better seen on less dense breast than a denser breast
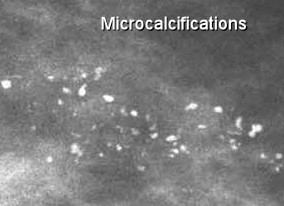
Suspicious clustered microcalcifications detected on MMG
Limitations of screening mammograms
Screening mammograms are also not 100% accurate in detecting cancer.
Approximately 15% of the screening report can be false negative or false positive resulting in unnecessary anxiety to the patient.
Guide to Mammography Reports – understanding BIRADS classification.
BI-RDAS stands for breast imaging reporting and data system.
This system is put in place to help the reporting radiologist or doctors to categorise the masses and communicate with the physician or surgeons regarding the mammographic findings.
The conclusion of the mammographic report will have a BIRADS assessment.
BIRADS Category
- Birads 0 : means incomplete assessment and further investigation with breast ultrasound is necessary to provide more information to ascertain the diagnosis.
- Birads 1 : Negative findings means no suspicious abnormalities found. Breast is clear.
- Birads 2 : Benign findings like well defined oval shaped mass , scattered macrocalcifications, vascular calcifications
- Birads 3 : Probably benign mass, unequivocal findings. Recommeded close follow up at 6 months and / or with furgher investigation like breast ultrasound.
- Birads 4 : Suspicious and indeterminate abnormality where risk of cancer is higher more than 60%. Further investigation with breast ultrasound and tissue biopsy is necessary to rule out possibility of malignancy.
- Birads 5 : Very high probability of malignancy where tissue biopsy is strongly advised to confirm diagnosis. Typical findings of category 5 presentations are malignant microcalcification, architectural distortion, ill defined and irregular margins, spiculated mass
- Birads 6 : Confirmed cancer from tissue biopsy
References:
- https://breast-cancer.ca/bi-rads/
- https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/mammograms/understanding-your-mammogram-report.html
